Primary Sjögren Syndrome Associated with Mixed Cryoglobulinaemia in Kidney Transplant Patient: A Case Report
Oscar Calle Mafla1, Rosario Cabello Jabalquinto3, Maria L Agüera Morales1, Alberto Rodriguez Benot1, Victoria E Garcia Montemayor1, Maria D Navarro Cabello1, Ana Martinez Lopez2, Pedro Aljama Garcia1.
1Nephrology, Hospital universitario Reina Sofia, Cordoba, Spain; 2 Pathology, Hospital universitario Reina Sofia, Cordoba, Spain; 3Medicine, Cordoba University, Cordoba, Spain
Mixed cryoglobulinaemia syndrome (MCS) has been rarely reported after kidney transplantation. In most patients, MCS is associated with chronic hepatitis C virus (HCV) infection. Among autoimmune diseases, primary Sjögren’s syndrome (SS) is the most frequent cause of mixed cryoglobulinaemia. Between 5 and 28% of patients with primary SS are seropositive for cryoglobulin.
A 59-year-old Spanish man, diagnosed of primary Sjögren´s syndrome for > 10 years with end-stage renal disease secondary to chronic tubulointerstitial nephritis, diagnosed by kidney biopsy, received a kidney graft in April of 2017 from a standard-criteria donor. In the first 24 hours after transplantation, he developed alveolar haemorrhage. Treatment with ventilation support, empirical antibiotherapy and bolus of steroids was satisfactory. At hospital discharge, good kidney graft function and creatinine of 1 mg / dL.
At 2-months post grafting he developed progressive decline of the allograft kidney function, creatinine 3.2 mg/dl, without clinical symptoms. Blood test showed low levels of C4 7.9 mg/dl, IgG 2910 mg/dl and rheumatoid factor 157. Serum cryoglobulins, previously negative, became positive at this moment.
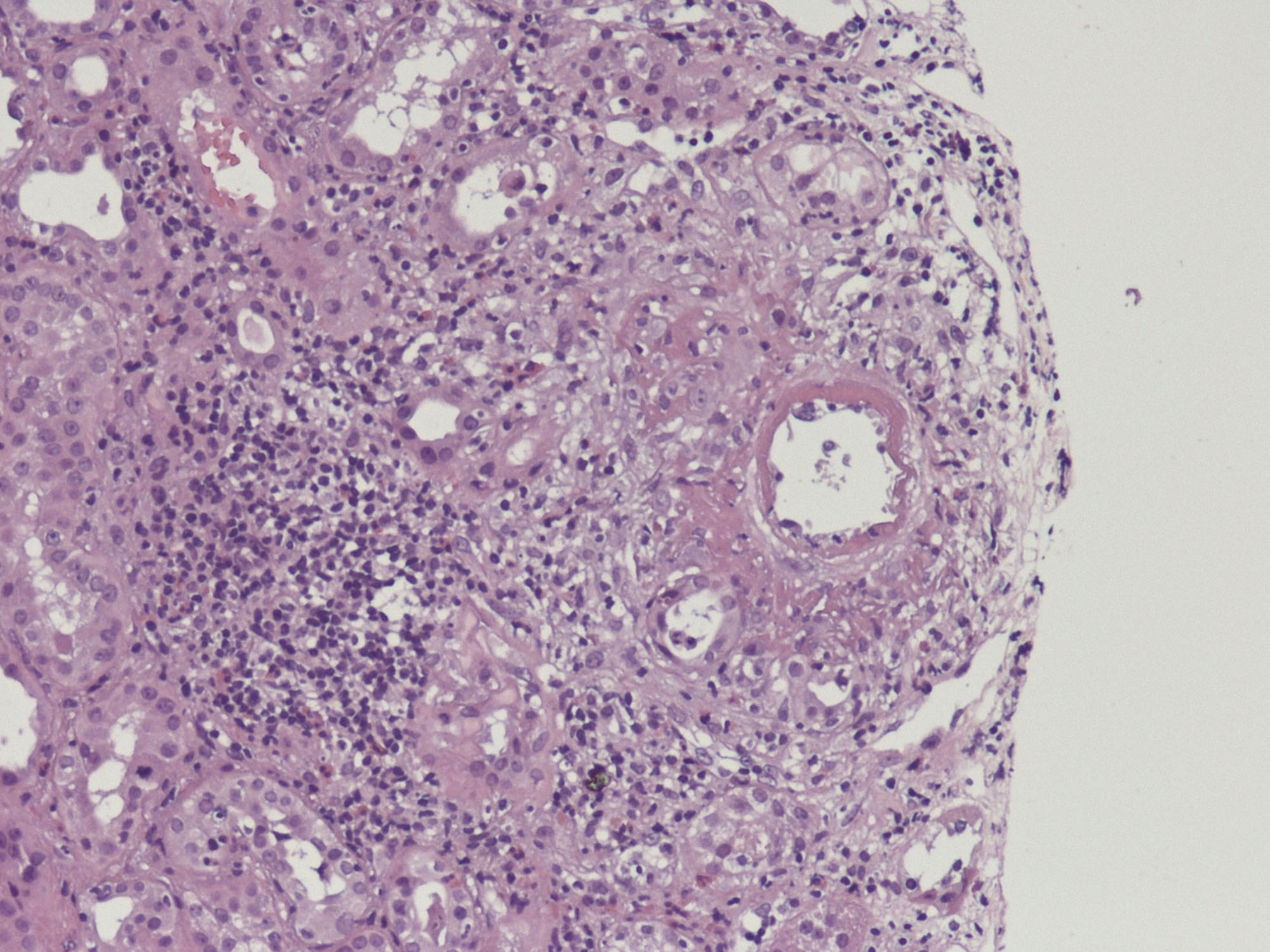
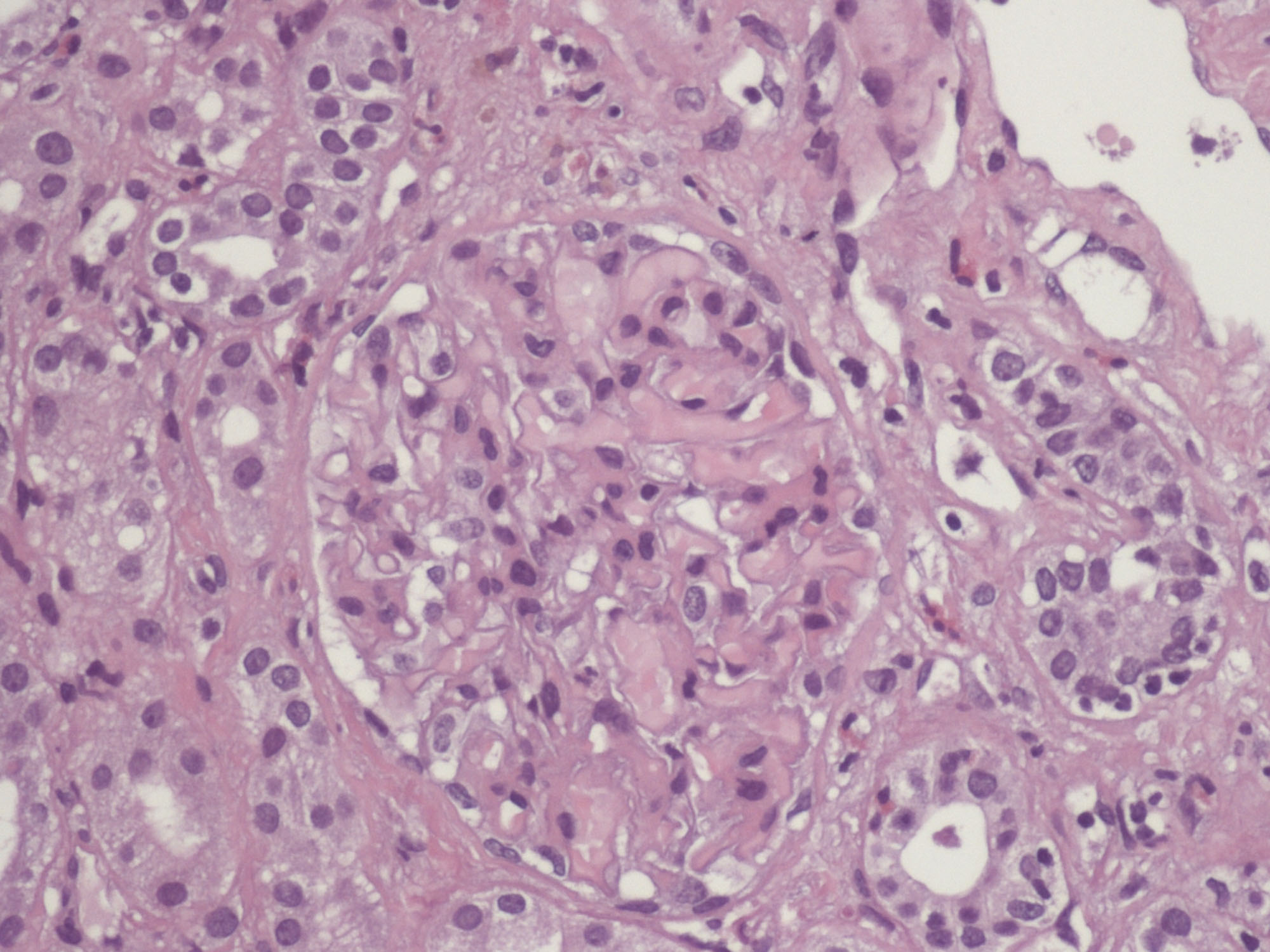
It was performed a kidney biopsy. Its study with optical microscope and immunofluorescence suggested acute allograft rejection mediated by T cells, mild to moderate intensity, as well as vascular involvement in one vessel (fibrinoid necrosis) and isolated glomerular microthrombus without evidence of humoral component (figure 1 and figure 2). The features of kidney biopsy, skin purpura and the blood test values made diagnose mixed cryoglobulinemic vasculitis. There was no response to high-dose steroid therapy, needing dialysis. After that, the patient was treated satisfactorily with 9 sessions of plasmapheresis but 10 days after the last session, cryoglobulins rebound. Rituximab and other B-cell-depleting therapies have to be reserved for refractory states. After treatment with rituximab, the allograft kidney function became better, with negative cryoglobulins and without needing dialysis.
Cryoglobulinemic vasculitis HCV related treated with rituximab generally produce favourable outcomes. A few studies suggest that renal and immunologic responses are better in the treatment with rituximab plus corticosteroids, with lower levels of corticosteroids in the maintenance. The long-term efficacy of cryoglobulinemic vasculitis treatment remains uncertain in patients with SS.
Cases with SS and kidney transplantation can develop decline of the allograft kidney function caused by cryoglobulins. Because of this, it is important to include MCS on the differential diagnosis of renal graft impairment in these patients.